Hereditary amyloidosis is one type of the systemic amyloidosis diseases that are caused by inheriting a gene mutation. That genetic mutation then produces an amyloid protein that forms into an abnormal shape. These abnormal “misfolded” amyloid proteins can be deposited and cluster in the body’s nerves and other organs and once they build up, this may affect and harm tissue and/or organ function. Even though you are born with a gene mutation, normally the harmful deposits don’t occur until adulthood. Although all the types of the hereditary amyloidosis can cause serious complications, there are some carriers of this genetic mutation that may not show symptoms of the disease at all. Others may have a few, more minor, health issues.
There are 2 main classifications of hereditary amyloidosis diseases: ATTR and Non-TTR.
However, it is further complicated by the fact that there are approximately 136 different genetic variations in ATTR, and at least 60 genetic variations in Non-TTR hereditary amyloidosis diseases. It is possible that more may be discovered as research continues. Each family with a certain hereditary form of amyloidosis has its own pattern of organ involvement, approximate age of onset and associated symptoms.
Typically, families know when they have a hereditary form of amyloidosis because of similar symptoms and causes of illness among blood relatives, so family history is a key indicator.
- ATTR Amyloidosis
ATTR Amyloidosis
ATTR amyloidosis means A for Amyloid and the TTR is short for the protein “transthyretin.” ATTR is one term that represents different kinds of mutations in a TTR gene that is inherited. That gene mutation makes the transthyretin unstable, so amyloid protein misfolding occurs. The amyloid fibrils then go out into the body and can damage nerves and/or organs, depending on the type of TTR mutation that the patient has inherited. TTR is mainly manufactured in the liver.
The majority of hereditary amyloidosis types are TTR-related, and there are many different variations within ATTR. Most ATTR diseases have a hereditary pattern of organ involvement, approximate age of onset and associated symptoms. It is common that symptoms do not appear until a person is an adult and the degree and severity of illness depends on the individual.
In the past, because ATTR often involves nerve or cardiac involvement, some terms were used when the chemical variations were less defined. Examples of these outdated terms include FAP (Familial Amyloid Polyneuropathy) and FAC (Familial Amyloid Cardiomyopathy).
Today, the different forms of ATTR are termed according to the “chemically based” name of the transthyretin protein variation. An example of this would be ATTRV30M (for ATTR Val30Met), which is the most common ATTR variation.
- Symptoms
Symptoms
If a patient has a clear family history along with clinical signs of amyloidosis, then ATTR is highly possible. However, there are times when someone is the first case to be identified in his or her family. Since many amyloidosis and other diseases can cause similar symptoms, it is vital that the patient is diagnosed properly with the type of amyloid protein clearly identified.
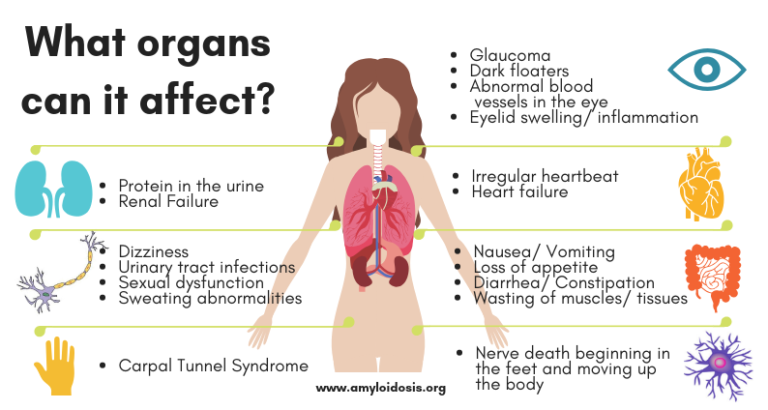
Symptoms of ATTR vary, depending on the TTR genetic variant that is involved and the organ (or multiple organs) that demonstrate signs of amyloid deposition. The most common sites of amyloid deposits are associated with cardiac and/or nerve involvement (called cardiomyopathy and neuropathy) and the gastrointestinal tract. The kidneys, eyes, and carpal ligament (also known as carpal tunnel syndrome) are among other possibilities that can be affected.
For each patient, the symptoms will depend on which organs are affected by the amyloid deposits. It also depends on the degree that the organ function is impaired.
The Heart
When amyloid deposits cause cardiomyopathy, it can result in a stiffening of the heart. Some patients may experience:
• Nausea
• Weight loss
• Inability to sleep
• Increasing fatigue
• Dizziness
• Shortness of breath
• Leg swelling (edema)
• Palpitations and abnormal heart rhythms (atrial fibrillation)
• Chest pain.Congestive heart failure and atrial fibrillation are the most common symptoms. The term “arrhythmia” refers to changes in the normal electrical impulses that cause the heart to beat. The result is a heart that can beat too fast, too slow or erratically. Atrial fibrillation (or a-fib for short) is one of the many forms of arrhythmia. During a-fib, the heart’s two small upper chambers cause an abnormal heart rhythm, usually rapid and irregular beating. This may result in increased heart damage, stroke or heart failure.
The Nervous System
The term neuropathy means nerve damage.
Peripheral Neuropathy
The following ATTR symptoms are caused by a condition known as peripheral neuropathy. Peripheral neuropathy (PN) can be caused by inflammation of, or damage to, the nerves. It can result in tingling, numbness and burning pain in any part of the body, but commonly is felt in the hands, feet and lower legs. Some patients may experience an increased sensitivity to pain. A loss of sensitivity to temperature may also occur. Sensorimotor impairment means the loss of a combination of sensory and motor activities. This can decrease a patient’s ability to move and feel (sensation) because of nerve damage. Restless leg syndrome (RLS) is also considered a sensorimotor disorder.Autonomic Neuropathy
Autonomic neuropathy (AN) is a condition that results from damage to nerves that assist in organ and organ system functioning. Autonomic nerves control the functions of our internal organs such as the heart, stomach and intestines, as well as the glands. Nerves affected by ATTR amyloid deposits may cause the inability to control the muscles that expand or contract blood vessels, which affects the heart rate (irregular heart beats) and blood pressure. If a patient has a sudden drop in blood pressure (such as when moving from a seated to a standing position), then dizziness, fainting, or lightheadedness may occur. Other body functions may also be affected, including perspiration patterns, poor digestion, bowel motility and erectile function.The Digestive System
The digestive system is also called the gastrointestinal tract (or GI tract). Amyloid deposits in the digestive system can affect the nerves that control intestinal muscle contractions causing nausea, diarrhea or constipation, and bladder control problems. Other symptoms may include weight loss, loss of appetite, or a feeling of fullness in the stomach after eating small amounts.
The Kidneys
Amyloid deposits in the kidneys can affect how they filter toxins and proteins in the blood. This may result in a condition called nephrotic syndrome, where there is excess protein in the urine and the lower legs can become swollen (also called “edema”). Swelling can affect the belly, arms, and lungs as well. In some cases, the amyloid deposits will cause the kidneys to lose the ability to purify the blood, which can lead to kidney failure; also known as “renal” failure. These patients may need dialysis to replace the function of the kidneys.
Other Symptoms
Swelling may develop and cause other symptoms as a result of the amyloid deposits. For example, patients may have carpal tunnel syndrome. This is when amyloid deposits in the wrist area squeeze and irritate the nerve, causing tingling and numbness in the fingers and thumb.
- Diagnosis
Diagnosis
First, a patient is tested to determine if they have amyloid proteins in their body. If amyloidosis is confirmed but the type is not clearly found in these tests, it will be important to do more tests to find the exact type and also to determine the variation of ATTR.
The main diagnostic testing for any amyloidosis disease includes blood tests, urine tests and biopsies. Some tests are only done once to confirm a diagnosis, while others may be repeated to monitor the disease and response to therapy.
Blood and urine tests will be done to help your doctor determine the diagnosis of amyloidosis. These tests can also help to show which organs are involved and how much damage they may have.
In addition, a tissue biopsy will be performed. This involves the removal of a small sample of tissue for lab examination. A tissue sample is essential to confirm the diagnosis and type of amyloidosis. A “Congo red stain” is put on the biopsy tissue and if the lab examiner then sees the light wave change to an apple green color (called “birefringence”) then amyloidosis is diagnosed.
With ATTR, after amyloidosis is confirmed and it is determined that there is transthyretin amyloid protein (via biopsy and Congo red staining in the lab), the protein needs to be identified by protein sequence analysis and DNA sequencing must be performed.
When scientists examine your blood for certain genetic markers it is called genome sequencing. A simple blood sample is sent to a lab and experts examine the DNA chains. If a certain condition is in question, then sections of the DNA chain will be checked for genetic markers of the condition or defect.
Since the hereditary amyloidosis variations affect individuals differently, it is important to establish which variation you have in order to identify a treatment plan that is tailored for your type of amyloidosis. The DNA sequence analysis of TTR identifies more than 99% of disease-causing mutations.
A person should never ignore any health problem. Early detection can be important with any disease and the more tests that are done, the more accurate the diagnosis.
- Treatment
Treatment
Today’s treatment plans are two-fold:
- Supportive treatment – treating your symptoms and organ damage
- Source treatment – slowing down, or stopping, the overproduction of amyloid at the source of the disease.
Supportive Treatment
Supportive treatment is helpful for various symptoms, including peripheral neuropathy, autonomic neuropathy, and cardiac and kidney problems, and can change the quality of life for many people. There are several medications that can be prescribed to treat peripheral neuropathy, which can cause tingling or burning in some parts of the body. These medications can help with pain relief and nerve damage. If a patient has autonomic neuropathy, symptoms can vary, with common problems affecting blood pressure, heart rate, digestion, and perspiration, depending on the location of the damage to the nerves. Other gastrointestinal dysfunctions may require treatment for symptoms that include poor nutritional health, diarrhea or constipation, and nausea or vomiting. Doctors can prescribe medications to help with these symptoms to lessen the pain and the symptom itself.
Management of heart problems, heart failure, and kidney dialysis (when needed) make a significant improvement on a patient’s quality of life. Reversing any damage to the organs and other parts of the body is difficult to achieve. If treatment begins during the early onset of clinical symptoms, the overall success rate is higher, so early detection is essential.
Source Treatment
For most ATTR variations, the liver is the main source of amyloid production. However, the liver itself is not affected by the disease in most cases and the amyloid burden causes damage in other parts of the body. A liver transplant is very helpful in reducing (or stopping) the amyloid deposits. It can stabilize or improve neurological symptoms as well as gastrointestinal problems (which can correct poor nutrition and overall health). However, the statistics vary as to who can benefit from these transplants, with the more common ATTR Val30Met having the highest success rate. The outcome of liver transplantation is largely dependent on the mutation that exists in the patient. In some cases, amyloid deposition does completely stop after transplantation, so research is ongoing in this area. For those patients with cardiac symptoms, studies have shown that heart problems may continue after a liver transplant. In some situations, a combined heart and liver transplant will help a patient with an ATTR variant that produces advanced cardiac problems. In 2019, two drugs were approved by the FDA for ATTR polyneuropathy of hereditary transthyretin-mediated (hATTR) amyloidosis in adults. The first was ONPATTRO (patisiran) lipid complex injection, a first of its kind RNA interference therapeutic. This drug aims to silence the gene expression. The second drug approved in 2019 is TEGSEDI which reduces the production of TTR protein through a once-a-week subcutaneous injection. In 2019, VYNDAQEL and VYNDAMAX were approved by the FDA for ATTR cardiomyopathy. These drugs are for oral administration taken once daily. In clinical trials, new therapies include aiming to treat the root cause of the disease, destabilized and folded TTR, using monoclonal antibodies to specifically target and clear misfolded (toxic) form a the TTR amyloid protein, and using a drug designed to reduce the production of transthyretin (TTR protein) in all types of TTR amyloidosis. Another RNA interference therapeutic is also currently in clinical trial. Advances in other treatments are likely, with new studies and clinical trials currently in view. It is possible that ATTR can cause serious health complications, so it should not be taken lightly. However, do not assume that disability or severe health issues are stamped on your future. There are treatments available and research continues.
- FAQ
FAQ
Why is it called ATTR?
Since systemic amyloidoses are referred to with a capital A (for amyloid) followed by an abbreviation for the fibril protein, ATTR amyloidosis stands for the protein transthyretin (TTR); so these diseases are often designated with the acronym ATTR.
TTR protein is something our body needs to function properly. In medical texts, transthyretin (formerly called prealbumin) is defined as a normal protein in the blood. In simpler terms, transthyretin helps to move the thyroid hormone and vitamin A (retinol) in your body. Thus, the name Transthyretin, which means that it TRANSports THYroxine and RETINol.
TTR is mainly manufactured in the liver; however a smaller portion also comes from the choroid plexus of the brain. Transthyretin goes into the blood from the liver, and the choroid plexus puts TTR into the cerebrospinal fluid.
What are the variations of ATTR?
There are more than 125 different TTR mutations that have been identified in ATTR. That means that within the one ATTR type, there exist many different variations, which are then identified by the amino acid protein involvement.
- The most common TTR variants in the United States are:
- Val30Met (also the most found worldwide). What was once termed FAP (Familial amyloid polyneuropathy) is most commonly caused by Val30Met.
- Thr60Ala
- Leu58His
- Ser77Tyr
- Val122Ile — predominantly seen in the African-American population; associated with cardiomyopathy (heart conditions). What was once termed FAC (Familial amyloid cardiomyopathy) is commonly caused by Val122lle.
Is it a form of cancer?
No. At this time, none of the types of amyloidosis diseases are considered to be cancer.
How does someone get ATTR or Non-TTR Hereditary Amyloidosis?
ATTR and Non-TTR are not contagious. They are considered to be an inherited, autosomal dominant disease. This means that to get this disease, a person needs one copy of the mutant gene – in other
words, it can be inherited from one parent. Each off spring of an affected parent has a 50/50 chance of inheriting the gene. If an offspring is not born with the gene mutation, then they can’t pass it onto their own offspring.How common is ATTR or Non-TTR Hereditary Amyloidosis?
ATTR and Non-TTR Amyloidosis can be found in virtually every ethnic background. Generally, they are an uncommon condition and are considered rare diseases, with some statistics estimating 1 per 100,000 of the population.
However, there is one ATTR type that alone puts the rare label in question. A variant named ATTR Val122lle is predominantly seen in the African-American population and it is associated with cardiomyopathy (heart conditions). What was once termed FAC (Familial amyloid cardiomyopathy) is commonly caused by ATTR Val122lle.
Medical statistics state that ATTR al122Ile is found in approximately 4% of the U.S. African-American population. That could mean that this gene mutation is carried by approximately 1.5 million people in the U.S.
This estimate is just the ATTR Val122Ile variation of hereditary amyloidosis and it is assumed that this variant is underdiagnosed. Remember, not everyone with the genetic mutation will experience symptoms, but this estimate takes the potential for carriers out of the rare category.
How does one gene mutation affect someone?
In simple terms, a gene is a segment of DNA that is coded to pass along a certain trait; it has a specific task (for example, determining the color of your eyes). Genes are building blocks that you inherit from your family.
The DNA sequence makes up a code that governs a particular cell’s function. A single gene on chromosome 18 is responsible for TTR genetic information. So, this gene mutation is one part of a DNA sequence and it can cause malfunctions.
Is a DNA test necessary?
One or more tissue biopsies are considered the most accurate diagnostic test available for all the amyloidosis diseases. When the tissue biopsy sample is stained with Congo red stain, it is then put under a light microscope and the amyloid deposits show up as an “apple green” birefringence (“birefringence” means double refraction) with the microscope in the lab.
Immunoassays are chemical tests done in a lab that are used to detect a specific protein or substance by using an antibody that is reactive with it. In this case, once the Congo red staining is performed and amyloid is confirmed, then additional immunoassaying of the biopsy specimen, using antiserum against TTR should also be performed.
However, this is not always enough. Since there are so many variations of hereditary amyloidosis, and more could be discovered, gene sequencing (a DNA test) is also necessary because immunoassaying may not identify a certain variant that is not within the more well known TTR types.
What is a “mutation”?
Genes are pieces of DNA, and most genes contain the information for making a specific protein. Some genes tell the body how to make a protein, for example, the TTR (transthyretin) gene tells the liver how to make the TTR protein. Sometimes there are differences in the coding of the gene so the body is told to make a slightly different protein.
This change is called a mutation in the genetic code of the DNA. DNA is isolated from a sample of blood, and then gene sequencing can be performed to see if a patient carries the genetic mutation for a particular variation of hereditary amyloidosis.
If there is a confirmed gene mutation, when might symptoms appear?
Most hereditary amyloidosis symptoms, if they develop, occur in adulthood. At that time, symptoms can range from none, to mild, to very severe. Although genetic tests can identify a particular problem gene, they cannot predict how severely that gene will affect the person who carries it.
If you are familiar with the common symptoms associated with your hereditary amyloidosis variant, you might be better able to keep a watchful eye on your health. For instance, you may not know that for some variations carpal tunnel syndrome can occur years before other symptoms develop. You could experience early signs of the clinical disease and not realize that there was a connection.
Having a genetic mutation is only a part of the story, because many illnesses develop from a mix of high-risk genes, environmental factors and/or unhealthy lifestyle (such as a smoker with a family history of familial cardiac amyloidosis). Make sure your doctor knows about the hereditary amyloidosis diseases, so they are able to monitor your health.
What is peripheral neuropathy and what are the symptoms?
Peripheral neuropathy (PN) can be caused by inflammation of, or damage to, the nerves. It can result in tingling, numbness and burning pain in any part of the body, but commonly is felt in the hands and feet.
What is autonomic neuropathy and what are the symptoms?
Autonomic neuropathy (AN) is a condition that results from damage to nerves that assist in organ and organ system functioning. Autonomic nerves control the functions of our internal organs such as the heart, stomach and intestines, as well as the glands. When your autonomic nerves are damaged, your blood pressure, heart rate, perspiration patterns, and bowel movements may be affected. In addition, you may have problems with dizziness, emptying your bladder, and/or experience gastrointestinal symptoms of diarrhea, weight loss, and poor digestion.
What if there aren’t any symptoms?
Your doctor will help you decide if you need a tissue biopsy if you have no clinical symptoms. It is important to understand that carrying the gene mutation does not always mean that you will have symptoms later on, or that this disease will seriously affect you.
If you have a parent with one of the hereditary amyloidosis types, you can be tested to see if you’ve inherited the same amyloid gene. This DNA test is done by a blood sample. If you suspect your parent has (or had) hereditary amyloidosis, but no definite diagnosis was ever made for this parent, try to speak to your parent’s doctor, or one of the doctors at the amyloid centers, in order to determine if testing is necessary.
What is the difference between DNA and RNA?
In simple terms, our DNA stores and transfers genetic information. A gene tells a cell how to make a specific protein. Proteins are formed inside our cells and it is our DNA that holds the “recipe” for making proteins.
DNA and RNA work together and they both carry genetic information to make up the many different proteins we need. However, they perform different functions for this task.
The RNA helps to move the DNA “code” from storage to where it can be used. RNA is converted (or “translated”) into a sequence of amino acids that makes up a protein.
In basic biological terms:
- Transcription = DNA → RNA
- Translation = RNA → protein
The collections of proteins within a cell are essential for our body’s health and function, and they work in a variety of ways, serving activity inside the cell as well as interaction outside the cell – in virtually every process within the cell.
How can the new RNAi research help with TTR amyloidosis diseases?
RNAi is short for “RNA interference.” By putting “silencing RNA” into cells that make an abnormal TTR, the translation of RNA to protein is stopped. This means that the production of the abnormal TTR that causes amyloid can be dramatically reduced. RNA interference technology is underway and shows promise. Whether it will change the course of patients with TTR amyloid is under active investigation now.
Is there a special diet that I can follow?
Eating a well-balanced, heart-healthy and nutritious diet is always recommended. Although amyloid is an abnormal protein, the amount of protein in the diet does not affect the onset of the disease. A diet low in protein and/or sodium may be necessary when the kidneys are involved. Consult with your physician on any dietary changes, and report any vitamins or other supplements that you take. You are a part of the team of people who must keep in communication with each other about your health.
What kind of doctor should be consulted?
It is strongly recommended that you consult with a specialist in the field of amyloidosis. The Amyloidosis Foundation provides a list of amyloidosis treatment centers under “Patient Resources” on this website. Once your diagnosis is confirmed, then a treatment plan can be laid out for your individual case. Depending on your symptoms, you will be seeing a local hematologist (blood), oncologist (cancer), neurologist (nerves), cardiologist (heart), nephrologist (kidney), gastroenterologist (GI tract), internist and/or general physician. These doctors should coordinate your care with the amyloidosis specialist to develop the best treatment program.
Would genetic counseling help?
If you have a family history of a certain variation of hereditary amyloidosis, then consult with your doctor. Seeking genetic counseling may be recommended, if you are an adult.
A genetic counselor is a specially trained professional who can help a patient with the process of deciding to test and identify family members who may have inherited a disease. They can help to investigate and examine any problems associated with the disease, interpret information to make it easier to understand, and help the patient and the family members review their options, while offering support in many areas.
Since genetic testing may contain emotional and physical significance for you and your family, this is a decision that, ultimately, you need to make for yourself. With a genetic counselor, once you have discussed the variety of issues surrounding the results of these types of tests, you can make an informed decision on whether to proceed with the testing process. Some people want to know if they carry a genetic mutation, so they can more carefully watch their health or understand the issues surrounding family planning.
However, it should be noted that many genetic counselors are not knowledgeable in the hereditary amyloidosis diseases, so your consultations with a qualified genetic counselor may only center on the broader issues of being tested for a genetically inherited disease. Regardless of your decision to be tested, medical professionals recommend that you acquaint yourself with the amyloid mutation that is identified within your family and know how to recognize the symptoms that generally accompany your hereditary amyloidosis variation.
Finding these problems early and treating them promptly might prevent future health complications, thus leading to improved quality of life.
What are the considerations before having a genetic test?
There are a number of personal, ethical, legal and social issues to think about. Apart from questions that are of a very personal nature, here are only some of the questions that you should ask a qualified genetic counselor, should you decide to see one:
- Who will have access to the information from the test results?
- How will that information be used?
- Who owns the genetic information stored in each individual’s DNA?
- Could testing lead to discrimination by employers or insurance companies, or to privacy and disclosure disputes?
- What is genetic discrimination?
- What are the ways that the results might change my life?
What are the insurance implications in the U.S.?
The Genetic Information Nondiscrimination Act of 2008, also referred to as GINA, is a Federal law that prohibits discrimination in health care coverage and employment based on genetic information. Some things to note about the GINA law:
- The law does not apply to employers with fewer than 15 employees.
- Employment protection does not apply to the US military.
- It does not apply to health insurance through the TRICAREmilitary health system, the Indian Health Service, the Veterans Health Administration, or the Federal Employees Health Benefits Program.
- GINA does not cover long-term care insurance, life insurance or disability insurance.
For more information, go to www.genome.gov
When discussing private insurance in the United States, the term “pre-existing condition” might be an issue. In the United States healthcare system, a pre-existing condition is a medical condition that started before a person’s health insurance went in to effect. If you sign up with the current Affordable Care Act, a health insurance company can’t refuse to cover you or charge you more just because you have a pre-existing condition.
One exception to this pre-existing coverage rule is with “grandfathered” private health insurance plans that you buy yourself, not through an employer. A grandfathered plan is an insurance plan that is in place on or before March 23, 2010 where the guidelines haven’t changed since they took effect. The insurance company must tell a consumer if their plan is grandfathered. These types of plans don’t have to cover pre-existing conditions. Some do, and some don’t – so read your coverage carefully. If you have one of these plans, you can switch to a plan through the Affordable Care Act that covers pre-existing conditions, if you think this will provide you with better insurance coverage.
For more information, go to www.healthcare.gov
Some patients with amyloidosis find it helpful to take out supplemental insurance at the appropriate time. There are some “critical illness” supplemental insurance plans that provide a patient with a cash benefit where cash can be used to cover lost wages, transportation or lodging related to your health condition, out-of-network specialists, or used to pay for food, medication, and other expenses that you may have due to a disease. With a condition like amyloidosis, traveling to get experienced health care can be necessary.
Regarding disability, if you start experiencing amyloidosis symptoms, and you live in the U.S., consider filing for social security disability (SSDI) to find out if you are entitled to receive such benefits. The application also includes a test for SSI eligibility, which is a special program for lower income persons that have not worked enough to earn social security benefits.
- Non-TTR Amyloidosis
Non-TTR Amyloidosis
These diseases are considered even more rare than the ATTR variations. The Non-TTR amyloidoses consist of other inherited gene mutations that can also cause major symptoms and affect your health. These proteins are Apo lipoprotein AI, Fibrinogen Aa, Lysozyme, Apo lipoprotein AII, Gelsolin, and Cystatin C. More variations may be discovered as research continues.
For example, in Europe and the United States, the most common Non-TTR proteins that cause kidney problems are Fibrinogen Aa and Apo lipoprotein AI. They are called this because of the mutations in the AFib and ApoAI genes.
- Symptoms
Symptoms
Non-TTR symptoms can vary with each mutation, including problems with the kidneys, liver, heart or peripheral neuropathy. Some mutations have symptoms that involve the brain or the eye.
Each individual can present with different clinical symptoms. The symptoms, as well as the prognosis, depend on the tissue and organ(s) affected by the amyloid deposits. Although all the hereditary amyloidoses may cause serious complications for some individuals, there are some carriers of genetic mutations that may not show symptoms of the disease at all. Others may have a few, more minor, health issues.
Like ATTR, there are numerous variations within the protein identification.
- Apolipoprotein AI – 22 known variations with differing symptoms, including amyloid deposit involvement in the kidneys, liver, heart, peripheral neuropathy, cutaneous (skin) areas, and laryngeal (larynx).
- Fibrinogen Aa – 14 variations with symptoms that only involve the kidneys, with 1 also involving neuropathy.
- Lysozyme – 7 variations that involve kidney and/or liver symptoms, with 1 also involving the GI tract.
- Apolipoprotein AII – 5 variations that involve kidney symptoms only.
- Gelsolin – 4 variations with peripheral neuropathy symptoms, 1 also involving the eye.
- Cystatin C – 1 variation with cerebral hemorrhage complications.
- Diagnosis
Diagnosis
First, a patient is tested to determine if they have amyloid proteins in their body. If amyloidosis is confirmed but the type is not clearly found in these tests, it will be important to do more tests to find the exact type and also to determine the variation of Non-TTR amyloidosis.
The main diagnostic testing for any amyloidosis disease is made up of blood tests, urine tests and biopsies. Some tests are only done once to confirm a diagnosis, while others may be repeated to monitor the disease and response to therapy.
Blood and urine tests will be done to help your doctor determine the diagnosis of amyloidosis. These tests can also help to show which organs are involved and how much damage they may have.
In addition, a tissue biopsy will be performed. This involves the removal of a small sample of tissue for lab examination. A tissue sample is essential to confirm the diagnosis and type of amyloidosis. A “Congo red stain” is put on the biopsy tissue and if the lab examiner then sees the light wave change to an apple green color (called “birefringence”) then amyloidosis is diagnosed.
With Non-TTR, after amyloidosis is confirmed and it is determined that there is amyloid protein (via biopsy and Congo red staining in the lab), the protein needs to be identified by protein sequence analysis and DNA sequencing must be performed.
When scientists examine your blood for certain genetic markers it is called genome sequencing. A simple blood sample is sent to a lab and experts examine the DNA chains. If a certain condition is in question, then sections of the DNA chain will be checked for genetic markers of the condition or defect.
Since these hereditary variations affect individuals differently, it is important to establish which variation you have in order to identify a treatment plan that is tailored for your type of amyloidosis. The genome sequencing does this. With the Non-TTR Amyloidosis diseases (AFib, ApoA1, ApoA2, ALys, etc.), it is highly recommended that the genome sequencing be performed or reviewed by one of the specialty amyloidosis centers in order to identify and verify the correct diagnosis.
A person should never ignore any health problem. Early detection can be important with any disease and the more tests that are done, the more accurate the diagnosis.
- Treatment
Treatment
Today’s treatment plans are two-fold:
- Supportive treatment – treating your symptoms and organ
damage; and, - Source treatment – slowing down, or stopping, the overproduction of amyloid at the source of the disease.
Supportive Treatment
Supportive treatment can vary with each mutation of the non-TTR diseases, however, many of them present with kidney or heart damage, so organ transplantation has been used in these cases with success. Although not a cure, and even if production of the variant amyloid protein continues, an organ transplant can slow the progression of the disease, improve quality of life and prolong survival significantly.
Source Treatment
Liver transplants are less of a source treatment option for most of the Non-TTR amyloidosis diseases. However, Fibrinogen is one variation that has amyloid production occurring solely in the liver, so a liver transplant can slow, or stop, amyloid production at the source. Often, a kidney transplant is also performed because kidney damage is the main target of this disease. So, transplants of both these organs can provide a successful supportive (kidney), and source (liver), treatment in this Fibrinogen variation.
Lysozyme, Apo lipoprotein A-I and AII, along with the other Non-TTR variations, are so varied that you should consult with a specialist at an amyloid center to recommend a treatment for your individual needs. Source treatments for the hereditary Non-TTR amyloidosis variants are not as advanced as they are for ATTR. These types are more rare and seem to progress slowly.
Current organ transplants and other treatments include:
Apolipoprotein AI
- Supportive Treatment Possibilities (affected organ) –
kidney and/or heart transplant, depending on organ damage - Source Treatment (to reduce amyloid production) – liver transplant
Fibrinogen Aa
- Supportive Treatment Possibilities (affected organ) –
kidney transplant - Source Treatment (to reduce amyloid production) – liver transplant
Lysozyme
- Supportive Treatment Possibilities (affected organ) –
kidney and/or liver transplant, depending on organ damage - Source Treatment (to reduce amyloid production) – none at this time
Apolipoprotein AII
- Supportive Treatment Possibilities (affected organ) –
kidney transplant - Source Treatment (to reduce amyloid production) – none at this time
Gelsolin
- Supportive Treatment Possibilities (affected organ) –
cornea transplant - Source Treatment (to reduce amyloid production) – none at this time
Cystatin C
- Supportive Treatment Possibilities – avoid fever
- Source Treatment (to reduce amyloid production) – none at this time
- Supportive treatment – treating your symptoms and organ
- FAQ
FAQ
Why is it called ATTR?
Since systemic amyloidoses are referred to with a capital A (for amyloid) followed by an abbreviation for the fibril protein, ATTR amyloidosis stands for the protein transthyretin (TTR); so these diseases are often designated with the acronym ATTR.
TTR protein is something our body needs to function properly. In medical texts, transthyretin (formerly called prealbumin) is defined as a normal protein in the blood. In simpler terms, transthyretin helps to move the thyroid hormone and vitamin A (retinol) in your body. Thus, the name Transthyretin, which means that it TRANSports THYroxine and RETINol.
TTR is mainly manufactured in the liver; however a smaller portion also comes from the choroid plexus of the brain. Transthyretin goes into the blood from the liver, and the choroid plexus puts TTR into the cerebrospinal fluid.
What are the variations of ATTR?
There are more than 125 different TTR mutations that have been identified in ATTR. That means that within the one ATTR type, there exist many different variations, which are then identified by the amino acid protein involvement.
- The most common TTR variants in the United States are:
- Val30Met (also the most found worldwide). What was once termed FAP (Familial amyloid polyneuropathy) is most commonly caused by Val30Met.
- Thr60Ala
- Leu58His
- Ser77Tyr
- Val122Ile — predominantly seen in the African-American population; associated with cardiomyopathy (heart conditions). What was once termed FAC (Familial amyloid cardiomyopathy) is commonly caused by Val122lle.
Is it a form of cancer?
No. At this time, none of the types of amyloidosis diseases are considered to be cancer.
How does someone get ATTR or Non-TTR Hereditary Amyloidosis?
ATTR and Non-TTR are not contagious. They are considered to be an inherited, autosomal dominant disease. This means that to get this disease, a person needs one copy of the mutant gene. In other
words, it can be inherited from one parent. Each off spring of an affected parent has a 50/50 chance of inheriting the gene. If an offspring is not born with the gene mutation, then they can’t pass it onto their own offspring.How common is ATTR or Non-TTR Hereditary Amyloidosis?
ATTR and Non-TTR Amyloidosis can be found in virtually every ethnic background. Generally, they are an uncommon condition and are considered rare diseases, with some statistics estimating 1 per 100,000 of the population.
However, there is one ATTR type that alone puts the rare label in question. A variant named ATTR Val122lle is predominantly seen in the African-American population and it is associated with cardiomyopathy (heart conditions). What was once termed FAC (Familial amyloid cardiomyopathy) is commonly caused by ATTR Val122lle.
Medical statistics state that ATTR al122Ile is found in approximately 4% of the U.S. African-American population. That could mean that this gene mutation is carried by approximately 1.5 million people in the U.S.
This estimate is just the ATTR Val122Ile variation of hereditary amyloidosis and it is assumed that this variant is underdiagnosed. Remember, not everyone with the genetic mutation will experience symptoms, but this estimate takes the potential for carriers out of the rare category.
How does one gene mutation affect someone?
In simple terms, a gene is a segment of DNA that is coded to pass along a certain trait; it has a specific task (for example, determining the color of your eyes). Genes are building blocks that you inherit from your family.
The DNA sequence makes up a code that governs a particular cell’s function. A single gene on chromosome 18 is responsible for TTR genetic information. So, this gene mutation is one part of a DNA sequence and it can cause malfunctions.
Is a DNA test necessary?
One or more tissue biopsies are considered the most accurate diagnostic test available for all the amyloidosis diseases. When the tissue biopsy sample is stained with Congo red stain, it is then put under a light microscope and the amyloid deposits show up as an “apple green” birefringence (“birefringence” means double refraction) with the microscope in the lab.
Immunoassays are chemical tests done in a lab that are used to detect a specific protein or substance by using an antibody that is reactive with it. In this case, once the Congo red staining is performed and amyloid is confirmed, then additional immunoassaying of the biopsy specimen, using antiserum against TTR should also be performed.
However, this is not always enough. Since there are so many variations of hereditary amyloidosis, and more could be discovered, gene sequencing (a DNA test) is also necessary because immunoassaying may not identify a certain variant that is not within the more well known TTR types.
What is a “mutation”?
Genes are pieces of DNA, and most genes contain the information for making a specific protein. Some genes tell the body how to make a protein, for example, the TTR (transthyretin) gene tells the liver how to make the TTR protein. Sometimes there are differences in the coding of the gene so the body is told to make a slightly different protein.
This change is called a mutation in the genetic code of the DNA. DNA is isolated from a sample of blood, and then gene sequencing can be performed to see if a patient carries the genetic mutation for a particular variation of hereditary amyloidosis.
If there is a confirmed gene mutation, when might symptoms appear?
Most hereditary amyloidosis symptoms, if they develop, occur in adulthood. At that time, symptoms can range from none, to mild, to very severe. Although genetic tests can identify a particular problem gene, they cannot predict how severely that gene will affect the person who carries it.
If you are familiar with the common symptoms associated with your hereditary amyloidosis variant, you might be better able to keep a watchful eye on your health. For instance, you may not know that for some variations carpal tunnel syndrome can occur years before other symptoms develop. You could experience early signs of the clinical disease and not realize that there was a connection.
Having a genetic mutation is only a part of the story, because many illnesses develop from a mix of high-risk genes, environmental factors and/or unhealthy lifestyle (such as a smoker with a family history of familial cardiac amyloidosis). Make sure your doctor knows about the hereditary amyloidosis diseases, so they are able to monitor your health.
What is peripheral neuropathy and what are the symptoms?
Peripheral neuropathy (PN) can be caused by inflammation of, or damage to, the nerves. It can result in tingling, numbness and burning pain in any part of the body, but commonly is felt in the hands and feet.
What is autonomic neuropathy and what are the symptoms?
Autonomic neuropathy (AN) is a condition that results from damage to nerves that assist in organ and organ system functioning. Autonomic nerves control the functions of our internal organs such as the heart, stomach and intestines, as well as the glands. When your autonomic nerves are damaged, your blood pressure, heart rate, perspiration patterns, and bowel movements may be affected. In addition, you may have problems with dizziness, emptying your bladder, and/or experience gastrointestinal symptoms of diarrhea, weight loss, and poor digestion.
What if there aren’t any symptoms?
Your doctor will help you decide if you need a tissue biopsy if you have no clinical symptoms. It is important to understand that carrying the gene mutation does not always mean that you will have symptoms later on, or that this disease will seriously affect you.
If you have a parent with one of the hereditary amyloidosis types, you can be tested to see if you’ve inherited the same amyloid gene. This DNA test is done by a blood sample. If you suspect your parent has (or had) hereditary amyloidosis, but no definite diagnosis was ever made for this parent, try to speak to your parent’s doctor, or one of the doctors at the amyloid centers, in order to determine if testing is necessary.
What is the difference between DNA and RNA?
In simple terms, our DNA stores and transfers genetic information. A gene tells a cell how to make a specific protein. Proteins are formed inside our cells and it is our DNA that holds the “recipe” for making proteins.
DNA and RNA work together and they both carry genetic information to make up the many different proteins we need. However, they perform different functions for this task.
The RNA helps to move the DNA “code” from storage to where it can be used. RNA is converted (or “translated”) into a sequence of amino acids that makes up a protein.
In basic biological terms:
- Transcription = DNA → RNA
- Translation = RNA → protein
The collections of proteins within a cell are essential for our body’s health and function, and they work in a variety of ways, serving activity inside the cell as well as interaction outside the cell – in virtually every process within the cell.
How can the new RNAi research help with TTR amyloidosis diseases?
RNAi is short for “RNA interference.” By putting “silencing RNA” into cells that make an abnormal TTR, the translation of RNA to protein is stopped. This means that the production of the abnormal TTR that causes amyloid can be dramatically reduced. RNA interference technology is underway and shows promise. Whether it will change the course of patients with TTR amyloid is under active investigation now.
Is there a special diet that I can follow?
Eating a well-balanced, heart-healthy and nutritious diet is always recommended. Although amyloid is an abnormal protein, the amount of protein in the diet does not affect the onset of the disease. A diet low in protein and/or sodium may be necessary when the kidneys are involved. Consult with your physician on any dietary changes, and report any vitamins or other supplements that you take. You are a part of the team of people who must keep in communication with each other about your health.
What kind of doctor should be consulted?
It is strongly recommended that you consult with a specialist in the field of amyloidosis. The Amyloidosis Foundation provides a list of amyloidosis treatment centers under “Patient Resources” on this website. Once your diagnosis is confirmed, then a treatment plan can be laid out for your individual case. Depending on your symptoms, you will be seeing a local hematologist (blood), oncologist (cancer), neurologist (nerves), cardiologist (heart), nephrologist (kidney), gastroenterologist (GI tract), internist and/or general physician. These doctors should coordinate your care with the amyloidosis specialist to develop the best treatment program.
Would genetic counseling help?
If you have a family history of a certain variation of hereditary amyloidosis, then consult with your doctor. Seeking genetic counseling may be recommended, if you are an adult.
A genetic counselor is a specially trained professional who can help a patient with the process of deciding to test and identify family members who may have inherited a disease. They can help to investigate and examine any problems associated with the disease, interpret information to make it easier to understand , and help the patient and the family members review their options, while offering support in many areas.
Since genetic testing may contain emotional and physical significance for you and your family, this is a decision that, ultimately, you need to make for yourself. With a genetic counselor, once you have discussed the variety of issues surrounding the results of these types of tests, you can make an informed decision on whether to proceed with the testing process. Some people want to know if they carry a genetic mutation, so they can more carefully watch their health or understand the issues surrounding family planning.
However, it should be noted that many genetic counselors are not knowledgeable in the hereditary amyloidosis diseases, so your consultations with a qualified genetic counselor may only center on the broader issues of being tested for a genetically inherited disease. Regardless of your decision to be tested, medical professionals recommend that you acquaint yourself with the amyloid mutation that is identified within your family and know how to recognize the symptoms that generally accompany your hereditary amyloidosis variation.
Finding these problems early and treating them promptly might prevent future health complications, thus leading to improved quality of life.
What are the considerations before having a genetic test?
There are a number of personal, ethical, legal and social issues to think about. Apart from questions that are of a very personal nature, here are only some of the questions that you should ask a qualified genetic counselor, should you decide to see one:
- Who will have access to the information from the test results?
- How will that information be used?
- Who owns the genetic information stored in each individual’s DNA?
- Could testing lead to discrimination by employers or insurance companies, or to privacy and disclosure disputes?
- What is genetic discrimination?
- What are the ways that the results might change my life?
What are the insurance implications in the U.S.?
The Genetic Information Nondiscrimination Act of 2008, also referred to as GINA, is a Federal law that prohibits discrimination in health care coverage and employment based on genetic information. Some things to note about the GINA law:
- The law does not apply to employers with fewer than 15 employees.
- Employment protection does not apply to the US military.
- It does not apply to health insurance through the TRICAREmilitary health system, the Indian Health Service, the Veterans Health Administration, or the Federal Employees Health Benefits Program.
- GINA does not cover long-term care insurance, life insurance or disability insurance.
For more information, go to www.genome.gov
When discussing private insurance in the United States, the term “pre-existing condition” might be an issue. In the United States healthcare system, a pre-existing condition is a medical condition that started before a person’s health insurance went in to effect. If you sign up with the current Affordable Care Act, a health insurance company can’t refuse to cover you or charge you more just because you have a pre-existing condition.
One exception to this pre-existing coverage rule is with “grandfathered” private health insurance plans that you buy yourself, not through an employer. A grandfathered plan is an insurance plan that is in place on or before March 23, 2010 where the guidelines haven’t changed since they took effect. The insurance company must tell a consumer if their plan is grandfathered. These types of plans don’t have to cover pre-existing conditions. Some do, and some don’t – so read your coverage carefully. If you have one of these plans, you can switch to a plan through the Affordable Care Act that covers pre-existing conditions, if you think this will provide you with better insurance coverage.
For more information, go to www.healthcare.gov
Some patients with amyloidosis find it helpful to take out supplemental insurance at the appropriate time. There are some “critical illness” supplemental insurance plans that provide a patient with a cash benefit where cash can be used to cover lost wages, transportation or lodging related to your health condition, out-of-network specialists, or used to pay for food, medication, and other expenses that you may have due to a disease. With a condition like amyloidosis, traveling to get experienced health care can be necessary.
Regarding disability, if you start experiencing amyloidosis symptoms, and you live in the U.S., consider filing for social security disability (SSDI) to find out if you are entitled to receive such benefits. The application also includes a test for SSI eligibility, which is a special program for lower income persons that have not worked enough to earn social security benefits.
